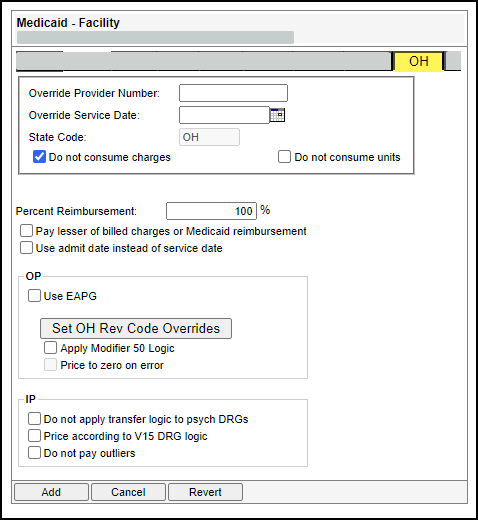
The following settings are either required or recommended for Ohio Medicaid managed care contracts.
- Override Provider Number – Type the preferred provider number.
- Override Provider Date – Type or select the override provider date.
- State Code – Defaults to OH (this value cannot be changed).
- Percent Reimbursement – This should be set to 100% unless specified otherwise. The Percent Reimbursement override is applied after the node calculations.
Note: Refer to the contract to determine the options to select and the values to enter.
The following table describes the fields on the OH tab of the Medicaid - Facility reimbursement tool.
Field | Description |
Override Provider Number | Preferred provider number. Up to ten alphanumeric digits. |
Override Service Date | Preferred service date. Use MM/DD/YYYY format. Overrides the service date on the claim with the date you enter. You may use the anchor date instead of this option. |
State Code | This field defaults to OH, and it cannot be changed. |
Do not consume charges | Provides the option not to consume charges. This is used for contract carve outs. |
Do not consume units | Provides the option not to consume units. This is used for contract carve outs. |
Percent Reimbursement | Three digit percentage amount. |
Pay lesser of billed charges or Medicaid reimbursement | Option to pay the lower amount of billed charges or calculated Medicaid reimbursement. |
Use admit date instead of service date | Provides the option to apply pricing logic by claim instead of by date of service. Ohio Medicaid treats each date of service as a separate claim. Note: Selecting this option allows managed care payors to apply the pricing logic to the entire claim instead of by date of service. |
OP | |
Use EAPG | Use the EAPG groupers to group and price claims. |
Set OH Revenue Code Overrides | This section allows you to enter percent overrides for specific revenue codes. To access the Set Revenue Code Overrides section, click Set Rev Code Overrides.
Note: This allows pass-throughs and carve outs in managed care contracts to use this reimbursement tool. |
Apply Modifier 50 Logic | Provides the option to apply to apply modifier 50 pricing when the facility is not billing detailed line items.
|
Price to zero on error | Enable (check) this option to include accounts that fail to price due to an error display with an expected reimbursement amount of zero ($0). When this check box is disabled (not checked), accounts price to 100% of billed charges. |
IP | |
Do not apply transfer logic to psych DRGs | Provides the option to allow the facility to ignore transfer logic on psych DRGs 425-435 and pay the full DRG instead.
Note: This is optional is for IP. It is not used for OP. |
Price according to V15 DRG logic | Provides the option to process claims based on the CMS V15 logic instead of the V15 DRG logic.
Note: This is optional is for IP. It is not used for OP. |
Do not pay outliers | Provides the option when you do not want outlier payments calculated on claims pricing against this contract profile.. This is used for contract carve outs. Note: This is optional is for IP. It is not used for OP. |