Note: Refer to the contract to determine the options to select and the values to enter.
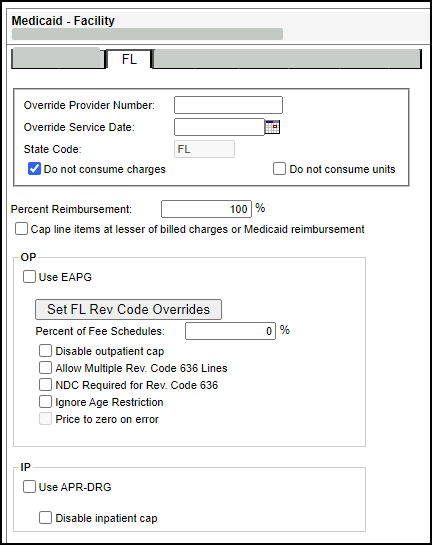
The following settings are required or recommended for Florida Medicaid managed care contracts:
- Override Provider Number – Type the preferred provider number (required).
- State Code – Defaults to FL (this value cannot be changed).
- Percent of Reimbursement – This should be set to 100% unless specified otherwise (required).
- Disable inpatient cap – Provides the option to ignore the day cap Medicaid places on inpatient claims (optional).
- Percent of Fee Schedules – Provides the option to calculate reimbursement as a set percentage of the Medicaid fee schedule amount (optional). Typically, this option is selected for managed care contracts that reimburse based on traditional Medicaid.
- Use APR DRG – Provides the option to calculate reimbursement using the All Patient Refined Diagnosis Related Group (APR-DRG) payment methodology.
Note: Typically, this option is only selected for managed care contracts that reimburse based on traditional Medicaid, but without the inpatient cap.
Note: The Percent of Reimbursement overrides the Percent of Fee Schedules. For example, if the Percent of Reimbursement is set at 105% the fee schedule rates would reimburse at 105%. This option is to be used only when labs or newborn hearing services are the only services that pay over or less than 100% of Medicaid reimbursement.
Note: This required ONLY if you want to reimburse using the APR DRG pricing logic.
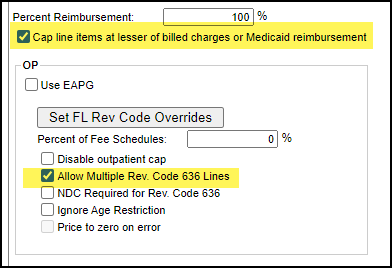
The Allow Multiple Rev. Code 636 Lines check box on the FL Medicaid Term Reimbursement Editor provides the option to allow multiple revenue code 0636 line items to reimburse per date of service.
- Click this check box to allow multiple revenue code 0636 line items to reimburse per date of service.
- Clear this check box to disallow multiple revenue code 0636 line items to reimburse per date of service.
Note: This box is checked by default.
Interactions between the Allow Multiple Rev. Code 636 Lines check box and the Cap line items at lesser of billed charges or Medicaid reimbursement check box are specified in the following four scenarios:
- All revenue code 636 lines are reimbursed at the lesser of billed charge for one unit or line item rate. This is the current behavior, no changes
- All revenue code 636 lines are reimbursed at the line item rate. This is the current behavior, no changes.
- Only one revenue code 636 line is reimbursed per service day at the lesser of billed charge for one unit or line item rate. The chosen line item is the one with the maximum billed charge among all revenue code 636 line items of the same day.
- Only one revenue code 636 line is reimbursed per service day at the line item rate. It does not matter which line is reimbursed because the line item rate is the same. However, to be consistent with scenario three, the line item with the maximum billed charge among all revenue code 636 line items of the same day will be reimbursed.
The following table describes the fields on the FL tab of the Medicaid - Facility reimbursement tool.
|
Field |
Description |
|
Override Provider Number |
Preferred provider number. Up to ten alphanumeric digits. |
|
Override Service Date |
Preferred service date. Use MM/DD/YYYY format. Overrides the service date on the claim with the date you enter. You may use the anchor date instead of this option. |
|
State Code |
This field defaults to FL, and it cannot be changed. |
|
Do not consume charges |
Provides the option not to consume charges. This is used for contract carve outs. |
|
Do not consume units |
Provides the option not to consume units. This is used for contract carve outs. |
|
Percent Reimbursement |
Three digit percentage amount. |
|
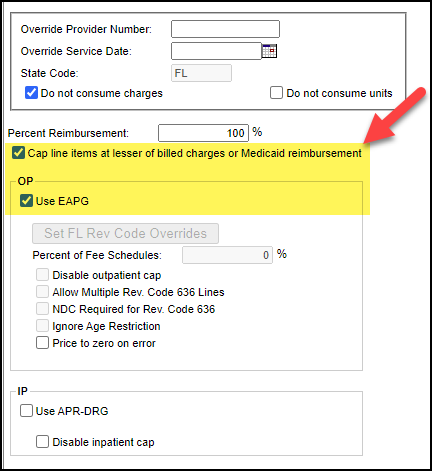
Cap line items at lesser of billed charges or Medicaid reimbursement |
Provides the option limit the calculated reimbursement at the line item level for outpatient claims to the lesser of the billed charges or the Medicaid reimbursement. Selecting this option ensures the calculated reimbursement never exceeds billed charges. |
|
OP |
|
|
Use EAPG |
Select to enable EAPG pricing. |
|
Set Revenue Code Overrides |
This section allows you to enter percent overrides for specific revenue codes. To access the Set Revenue Code Overrides section, click Set Rev Code Overrides.
Note: This allows pass-throughs and carve outs in managed care contracts to use this reimbursement tool. |
|
Percent of Fee Schedules |
Provides the option to calculate reimbursement as a set percentage of the Medicaid fee schedule amount. For example, the user can specify reimbursement as 105% of the Medicaid rate. Typically, this option is selected for managed care contracts that reimburse based on traditional Medicaid. |
|
Disable outpatient cap |
Provides the option to ignore the monetary cap Florida Medicaid places on outpatient claims. Typically, this option is only selected for managed care contracts that reimburse based on traditional Florida Medicaid, but without the outpatient cap. |
|
Allow Multiple Rev. Code 636 Lines |
Provides the option to allow multiple revenue code 636 line items to reimburse per date of service.
Note: This box is checked by default. |
|
NDC Required for Rev Code 636 |
Provides the option to require a valid NDC code to price revenue code 636 line items on OP claims. This option works in conjunction with Allow Multiple Rev. Code 636 Lines:
|
|
Ignore Age Restriction |
Provides the option to ignore the Newborn Hearing Age restriction for claims with Rev Code 0471 and CPT Codes 92585-92588 if the patient is older than 12 months . |
|
Price to zero on error |
Enable (check) this option to include accounts that fail to price due to an error display with an expected reimbursement amount of zero ($0). When this check box is disabled (not checked), accounts price to 100% of billed charges. |
|
IP |
|
|
Use APR-DRG |
Provides the option to calculate reimbursement using the All Patient Refined Diagnosis Related Group (APR-DRG) payment methodology. Note: Implemented by Florida Medicaid beginning 07/01/ 2013. |
|
Disable inpatient cap |
Provides the option to ignore the day cap Medicaid places on inpatient claims. Typically, this option is only selected for managed care contracts that reimburse based on traditional Medicaid, but without the inpatient cap. |