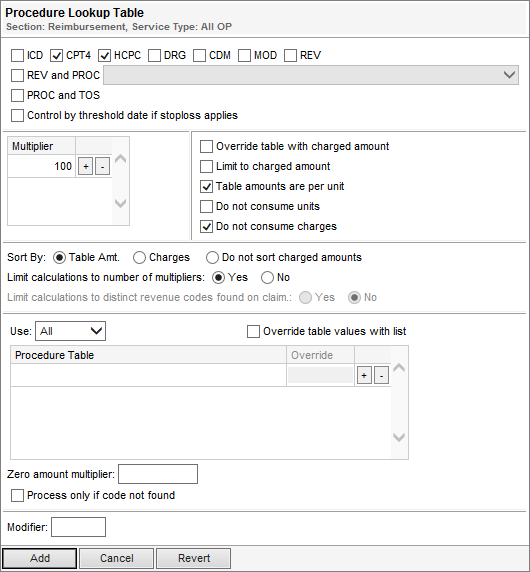
Procedure Lookup Table
The Procedure Lookup Table tool is useful in calculating reimbursement for codes in one or more procedure lookup tables.
Important distinctions about this tool is it can reference the following code types:
- ICD9
- ICD10
- CPT4
- HCPC
- DRG
- CDM
- Revenue
Note: Cannot reference a modifier lookup table or DRG weight table.

- Make sure you select the code type that reflects the referenced table(s)’ code type. The system does not report an error when the selected code type does not correspond to the contents of the table(s).
- If you do not select the code type that is found in the referenced table(s), the tool calculates reimbursement as $0.00.
- If you select a code type in addition to what is found in the referenced table(s), the tool can calculate multiple reimbursement amounts.
- Selecting/clearing CPT4 or HCPC automatically selects/clears the other option.
- If you select REV and PROC, make sure no other code type is selected.
- If you select REV, you can choose to limit calculations to distinct revenue codes. This means the reimbursement tool will limit reimbursement to unique codes when duplicate revenue codes are found on a claim.
- In Multiplier and Zero amount multiplier, do not convert whole percentages into decimals. For example, for 80%, type 80; If you type .80, the system calculates .8%.
- The Multiplier(s) does not reference units; it only references charges.
- For outpatient surgery reimbursement, you typically clear the Table amounts are per unit option.
- Make sure you set the Limit calculations to number of multipliers option appropriately. The default is Yes.
- When selecting a table, make sure you select the right table with the right code type.
- All Universal tables and tables in your facility are available.
Note: See Lookup Tool vs. Code Tool for a comparison between the the Procedure Lookup Table tool (Lookup tool) or the Procedure Code Reimbursement tool (Code tool).
The following table describes the fields on the Procedure Lookup Table tool.
Field | Description |
CDM | For claims with CDM codes |
Code Types | Code type(s) that reflects the code type of the procedure lookup table used in the tool. Except for CPT4 and HCPC, you typically do not select more than one at a time |
Control by threshold date if stoploss applies | Provides the option to calculate procedure code reimbursement by counting the procedure code lookup items to the second dollar stop loss threshold day rather than the entire length of stay. This check box is ignored if the claim does not qualify for stop loss. Note: This option is only available if you selected the ICD9 check box. |
CPT4 | For claims with CPT4 codes. Always selected in conjunction with HCPC |
Do not consume charges | Provides the option not to consume charges. This is used for contract carve outs. |
Do not consume units | Provides the option not to consume units. This is used for contract carve outs. |
DRG | For claims with DRG codes. This references a procedure lookup table that contains DRG codes–it does not reference a DRG weight table |
HCPC | For claims with HCPC codes. Always selected in conjunction with CPT4 |
ICD9 | For claims with ICD9 codes. When selected, some options are unavailable |
Limit calculations to distinct revenue codes found on a claim | Determines whether duplicate revenue codes are reimbursed:
Note: This option is only active if you select the REV check box at the top of the reimbursement tool. |
Limit calculations to number of multipliers | Determines the number of procedures to reimburse:
|
Limit to charged amount | When selected, limits the reimbursement to the charged amount per line item |
For claims with modifiers. When selected, the system refers to Modifier for instruction (refer to the Modifier description). | |
Used in conjunction with the MOD option (in the code types section)
Note: When using modifiers, the Procedure Code Reimbursement tool is recommended. | |
Multiplier | Percentage applied to the reimbursement |
Override | Dollar value applied to the selected table; when Override table values with list is selected, the values in this column override the values in the selected table |
Override table values with list | When selected, overrides the table’s base amount(s) with the value(s) listed in the Override column Note: It is useful for ASC groupers to use one table across multiple contracts. |
Override table with charged amount | When selected, overrides the table’s base amount with the charged amount for each code |
PROC and TOS | For facilities (Pennsylvania Medicaid only) that bill with TOS (type of service) codes |
Procedure Table | Procedure lookup table(s) and/or fee schedule(s) used in calculating reimbursement. The list includes Universal tables and all procedure lookup tables in your facility |
Process only if code not found | When selected, applies the Zero amount multiplier to codes that are not found in the table |
REV | For claims with revenue codes. For claims with revenue codes and procedure codes on the same line, use REV and PROC |
REV and PROC | For claims that include the revenue code and procedure code on the same line
|
Sort By | Determines the order of reimbursement:
|
Table amounts are per unit | When selected, calculates reimbursement based on units associated with each code. When not selected, calculates reimbursement based on the day. For example, if a procedure is performed two or more times on the same date, and this check box is not selected, the procedure is only paid once. |
Use | For duplicate codes in multiple tables, indicates which code to reimburse:
|
Zero amount multiplier | For codes with a base price of zero, applies the entered amount as a percentage to the code charges (when Process only if code not found is cleared) |