Pricing Transparency
Hospital pricing transparency (required by law starting January 1, 2021) is to provide a machine-readable file that includes the cost of a hospital item or service allowing consumers the ability to estimate the cost of care prior to a hospital stay or visit.
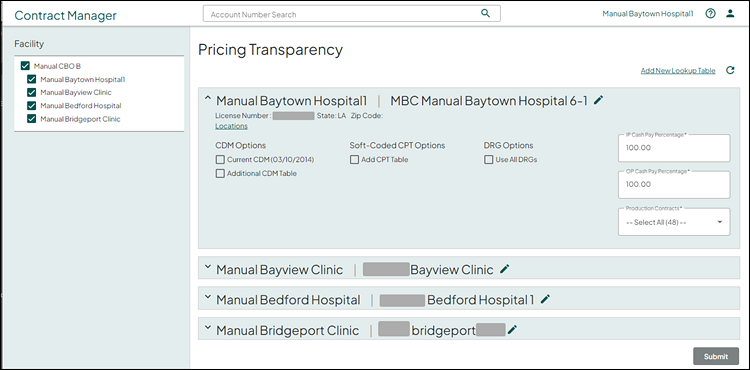
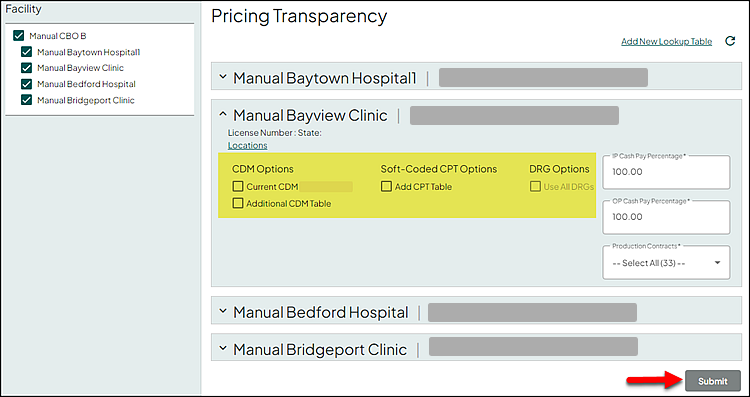
Contract Manager provides a reporting feature allowing you to select the parameters and generate your facility's pricing transparency machine-readable file. The facilities displayed on the left hand side of this page are based your facility access, and if the facility has the facility flag: Pricing Transparency, set to Y.
Select Go To > Pricing Transparency.
The Facility and associated facilities display on the far left.
- Make sure that all facilities to be included in the output file are checked (selected)
- For any facility that should not be included in the output file, remove the check (unselect)
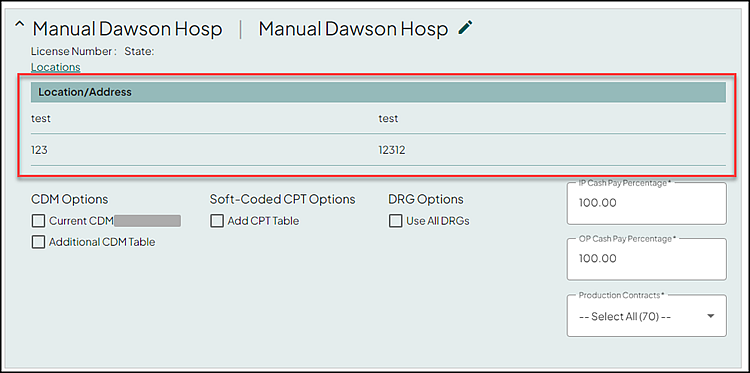
For each selected facility, an expandable section for each facility displays in the main part of the page. Use the expander to do the following:
- Open a specific facility section to display heading (license number, state, locations when applicable) and output file parameters
- Close the facility section after viewing, or updating heading and output file parameters
In the following example, all of the facilities are selected on the right. The first facility selected is in the expanded mode in the main part of the screen and displays the current output file parameters.
Note: Expand the facility section to view and/or update the output file parameters.
(Optional) To add a new table, click Add New Lookup Table. This action opens the Lookup Table Management page (see Manage Lookup Tables for additional information). At any time, click the refresh icon to refresh the table drop down lists.
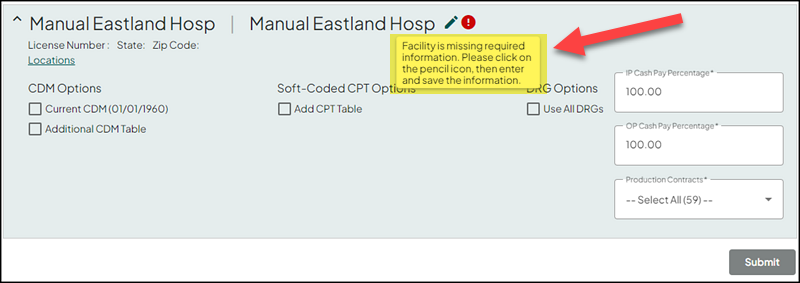
All of the location fields are required. You are prompted with the following message when any of the information is missing.
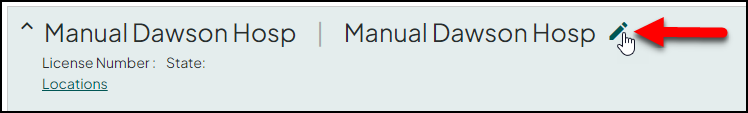
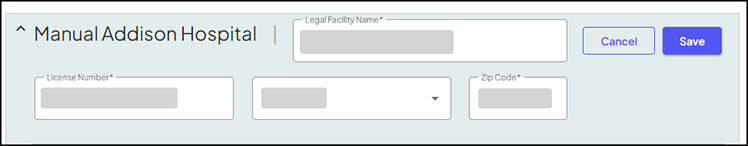
Click the pencil icon to the right of the facility name to view or edit heading information.
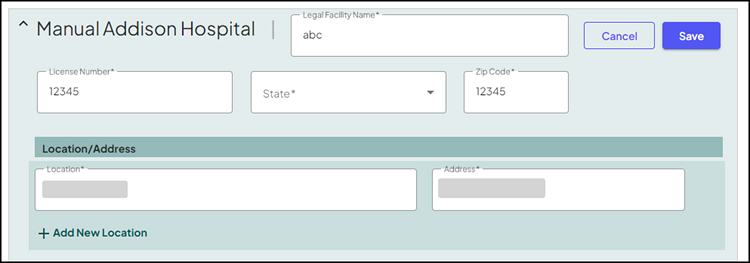
The above action expands with additional fields. Make the appropriate updates to any of the following fields:
-
Legal Facility Name - the information entered in this text box displays within the heading of the report. Enter/update with the appropriate information as needed.
-
License Number - the information entered in this text box displays within the heading of the report. Enter/update with the appropriate information as needed.
-
State - the information selected from this drop down list displays within the heading of the report. Select/update with the appropriate information as needed.
-
Zip Code - the information entered in this text box displays within the heading of the report. Enter/update with the appropriate information as needed.
Note: For professional facilities, the systems uses the zip code entered for specific carrier/locality look-ups.
-
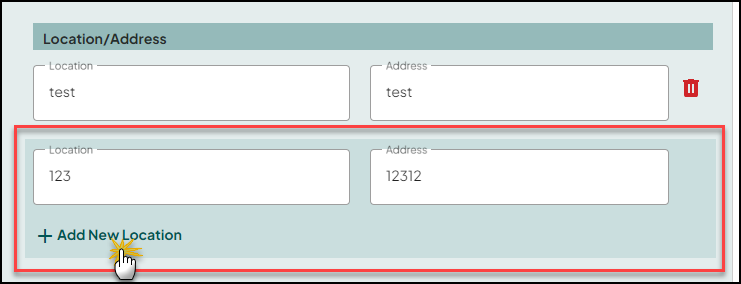
Location/Address section
-
Location - the information entered in this text box displays within the heading of the report. Enter/update with the appropriate information as needed.
-
Address - the information entered in this text box displays within the heading of the report. Enter/update with the appropriate information as needed.
-
Trash Can icon - use to remove a specific location/address from the selected facility.
-
(Optional) Use the Add New Location section to add an additional location address.
-
Enter the Location and Address in the appropriate fields
-
Click Add New Location
Click Save to commit your updates. Or click Cancel to return to the previous information without saving your changes.
Note: If any the following output file parameters are selected, heading editing is disabled.
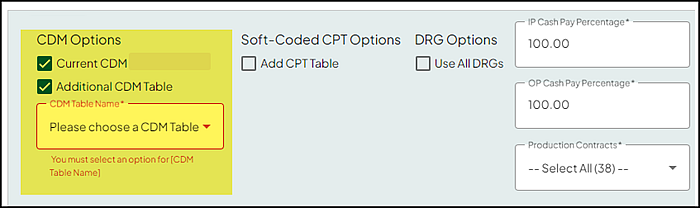
In the CDM Options section, use the following to make the appropriate CDM table selection.
- Current CDM (includes the date of last import) - select this check box to use the current CDM table/information.
- Additional CDM Table - select this check box to use an additional CDM Table. Make the appropriate selection from the CDM Table Name drop down list.
Note: During the CDM table import process, any special characters (“'\!@#$%^&*+={}[]|:;?`~") in the description column are replaced with a space and any description over 50 characters is truncated to 50 characters. See Import Lookup Table Data from a Text File for additional information.
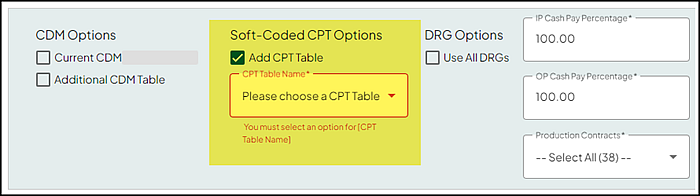
In the Soft-Coded CPT Options section, use the Add CPT Table check box to select CPT codes not included in the CDM file either by billed CPTs or by the CPT table (loaded into the look up table service).
Note: The CPT descriptions are pulled from a MDM database that is up to date with any CMS updates.
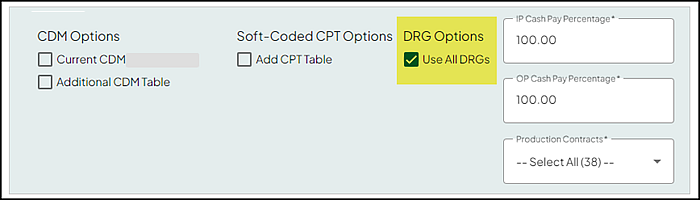
In the DRG Options section, select the Use All DRGs check box to select All DRG codes or billed DRG codes from the prior year:
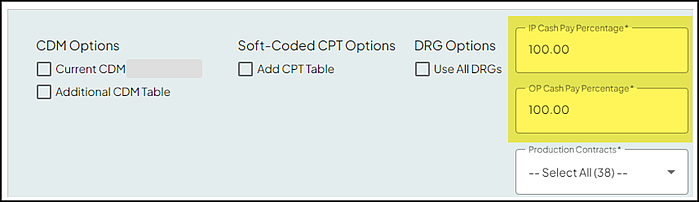
Enter the appropriate value for the following:
- IP Cash Pay Percentage - defaults to 100.
- OP Cash Pay Percentage - defaults to 100.
Note: Only values between 0 and 100 are valid. You are prompted with an error message for any value out side of this range, including negative numbers.
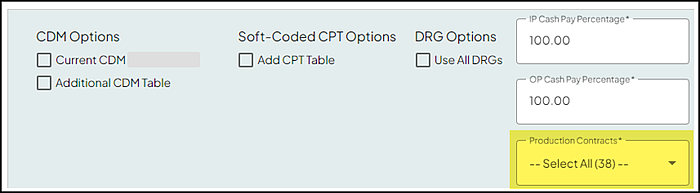
The Production Contract field defaults to the Select All option (the number in parentheses indicates the number of selected contracts). Make the appropriate selection(s) as needed. Multiple contracts can be selected.
Note: Your contract selections for each facility are saved and automatically selected by default in each report. These selections persist across sessions, and any changes are immediately reflected for the corresponding facility.
If additional facilities are selected on the left, you must expand each facility and make the appropriate CDM table, CPTs, and DRGs selections prior to submitting the report request. Until each facility is reviewed and appropriate selections made, the Submit button is disabled (grayed out).
Click Submit to generate the file.
Note: If the CDM Table, CPTs, and DRGs options are all set to None, the Submit button is not available. You must make the appropriate selection or selections to submit the report request.
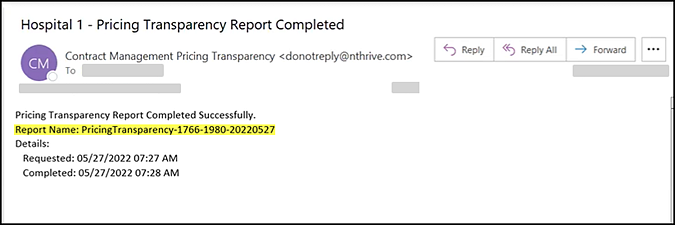
An email notification is sent once the request is complete and includes the report name.
See Search for Reports for additional information on viewing and downloading the report.
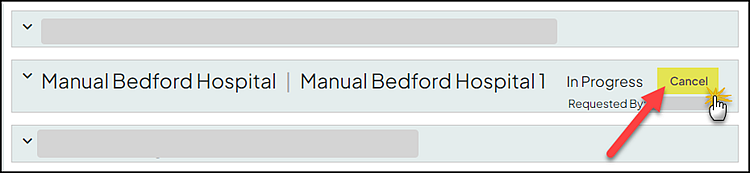
If you need to cancel a pricing transparency report request (i.e. you need to change the criteria), click Cancel on the right.
Note: The Cancel option is only available when the request is Queued or In Progress. You cannot cancel once the request is completed.
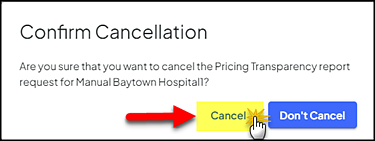
This action opens the Confirm Cancellation message prompt. Click Cancel.
Pricing Transparency includes the following for CDM Inpatient (IP) line items:
-
CDM line items 022-219 are for Inpatient (IP) only and are not included in outpatient OP.
-
If the contract is simple percentage, only a percentage calculation is applied to all lines on the report.
-
If the contract percent of charge is the only reimbursement term in that default service type, then all IP lines for the contract are processed through the pricer.
-
If the contract includes IP/All patient type Pass Throughs, IP lines with revenue codes 274, 275, 276, 278, and 636 are processed through the pricer.
-
Any other IP CDM lines display N/A on the report.
The Pricing Transparency report heading includes the following information:
-
Hospital/Facility Name*
-
File Run Date
-
Version (displays 2.0.0)
-
Location*
-
Address*
-
License Number*
-
Payor name
-
Contract profile name
-
Acknowledgment statement - “To the best of its knowledge and belief, the hospital has included all applicable standard charge information in accordance with the requirements of 45 CFR 180.50, and the information encoded is true, accurate, and complete as of the date indicated”.
Note: *The facility location information (location name, location, address, state, and license number) are populated using information from the Pricing Transparency page into row two when the report is created. See Edit facility name, license number, state, and location(s) for additional information.
The report includes the following columns:
-
description
-
code|[i] (increases with more codes)
-
code|[i]|type ( increases with more codes and displays CDM, RC, CPT, HCPCS, MS-DRG, APR-DRG, APC, EAPG, NDC, ICD)
-
modifiers (individual modifier lines include modifier, description, negotiated percentage, and the additional payer notes display the reimbursement text with the percentage)
-
setting (displays either inpatient , outpatient, or both)
-
billing_class (displays either facility or professional)
-
drug_unit_of_measurement
-
drug_type_of_measurement
-
standard_charge|gross
-
standard_charge|discounted_cash
-
standard_charge|min
-
standard_charge|max
-
additional_generic_notes
-
standard_charge|[payer_name]|[plan_name]|negotiated_dollar
-
standard_charge|[payer_name]|[plan_name]|negotiated_percentage
-
DRGs or soft-coded CPTs that do not have a standard charge amount and are reimbursed as a percentage, this field is populated with that percentage.
-
-
standard_charge|[payer_name]|[plan_name]|negotiated_algorithm
-
Displays the Level of Care (LOC) for any service type loaded with a LOC value.
-
-
standard_charge|[payer_name]|[plan_name]|methodology
-
Case Rate displays when the reimbursement is DRG Lookup, DRG, Flat, or Procedure Lookup (PLT, PLT2, and CPE) with rate (no percent). Also, Case Rate displays for contracts with DRG Weight * Base Rate followed by If: Current Amount = 0.00.
-
Fee Schedule displays when the reimbursement is Procedure Lookup with % of Table, Medicare OP, Tricare OP, WC OP, Medicaid OP, or Daily Charge grouper with Fee Schedule
-
Per Diem displays when the reimbursement is Per Diem, Formula/FormulaCPE: Days in Service Type, Formula/FormulaCPE: Days In Visit, or Daily Charge Grouper with a flat amount (because it pays the flat amount per day)
-
Percentage of Total Billed Charge displays when the reimbursement is Percent of Charges in Service Type, Percent of Gross Charges Adjusted, Formula or FormulaCPE: Charges in Service Type - (Charges in Exclusion Section + Charges in Pass Through Section) * %
-
Other displays for any other reimbursement terms when none of the above apply.
-
-
estimated_amount|[payer_name]|[plan_name] displays the estimated amount for all DRGs, or when the methodology for an inpatient ICD-10, or outpatient CPT line is either Other or Percent of Billed Charges. The estimated amount is calculated using instances with a specific code within the past 365 days. If there are one or more instances, the average amount for that code is calculated and recorded in the estimated_amount field, along with a note indicating One or more instances of the item or service in the 12 months prior to posting the file. Conversely, if there are no instances, the estimated_amount field remains blank, and a note is added indicating Zero instances of the item or service in the 12 months prior to posting the file.
-
additional_payer_notes|[payer_name]|[plan_name]
-
When the Method is equal to Other, the reimbursement text from the associated Contract Profile is populated into the additional payer note field.
-
If the line item is a Pass-Through service type, Payable in addition to (inpatient/outpatient) services is added.
-
Note: Terms loaded in the service type are added to the additional payer notes.
Pseudo claims are currently and previously created based on the lines in the CDM, a list of DRGs, or soft-coded CPT as the only code on the claim. That leaves a gap for the service types that are defined by having multiple code|code type requirements such as an age factor or ER when billed with Observation, or a claim level requirement such as a bill type or ICD10 code.
Note: Service types with tokens for ICD only in the condition expression do not display the Services not Matched Report.
Since Contract Manager allows flexibility with contract loading, these scenarios need to be reviewed to determine the best way to map and price services that are not automatically created by the above mentioned files. In the interim, all service types are tracked in the contract profile and a file is created for any service type without a match. You need to review and decide how to best manually add these to the report.
This report includes the following for service types without a match:
-
Contract Profile Name
-
Service Type
-
Condition Expression
-
Reimbursement Text
Note: When all service types are matched during pricing, the above report is not generated.
If hospital contracts with a professional service type are loaded in the Contract Profile, then for every CDM with a CPT/HCPCS code or Soft-Coded CPT code, these are sent through the pricer on a HCFA claim to determine the reimbursement amount. If no reimbursement amount is present across any of the contract profiles, these lines are not included in the report for the professional setting.