Create a Patient List from Bills
The Create Patient List (from Bills) page allows you to define a list of accounts based on bill data, according to specified criteria. That patient list can then be used in a model to reprice the patient list accounts in specific scenarios.
- Access the Create Patient List (from Bills) page:
- Select Go To > Contract Modeling > Advanced Contract Modeling. The Contract Modeling page opens.
- Select the Patient Lists tab.
- Click Create Patient List From Bills. The Create Patient List (from Bills) page opens. Type a name for the patient list in the Name field.
- Click each facility you want to include in your patient list to move it to the Selected facilities column.
- Enter the criteria used to identify accounts to include in your patient list.
- Click Add in the Criteria section. The Add Criteria window opens and displays a list of all available criteria.
- To add a criteria to your patient list, click the criteria field name.
- When you click a field name, the field name is added to the Selected Field Names list.
- To remove the criteria from your patient list, click the field name in the Selected Field Names list. The criteria is moved back to the list of available field names.
- You can add multiple date criteria, including multiple criteria of the same type, but you can only select one Contract or Product criteria for your patient list.
- You can also search for a specific criteria by typing the field name in the Search field. For example, to search for Admission Date, type Adm in the Search field.
- You can also limit the list of criteria by category, such as date. For example, to limit the list to field names related to dates, type Date in the Search field.
- For more information about a specific criteria, refer to the Field Descriptions table below.
- When you have selected all of the criteria you want to add to your patient list, click Apply. The Add Criteria window closes, and your selected criteria display in the Criteria section.
- Define the specific values for each criteria.
- Most criteria include an operator list that allows you to select an operator, such as Equals, Less Than, Greater Than, and so on, in addition to the value field. For example, you can select a hospital service code that equals "1234".
- For more information about creating complex, contract-based, or product-based patient list criteria, refer to the following:
- To remove a criteria, click
 next to the criteria.
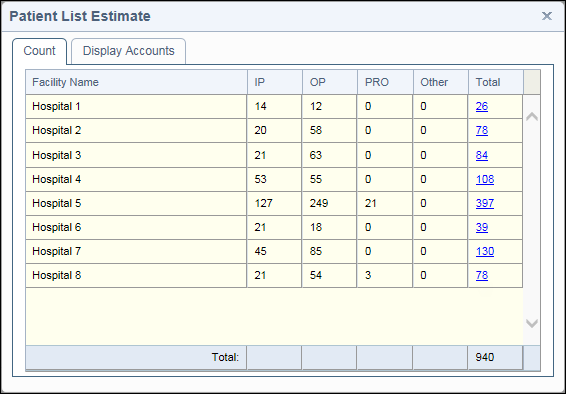
next to the criteria. - To see an estimate of how many accounts your patient list would include before you save it, click Estimate. The Patient List Estimate page opens and displays the number of accounts for the patient list, by facility.
Note: Use a name that allows you to easily identify the patient list. This is the name that appears in the list of available patient lists when creating a model.
Note: To remove a facility, click the facility name in the Selected facilities column.
Note: To clear all of the criteria you created and return the patient list to the default criteria, click Clear All.
- Review the estimate of accounts.
- Click the Account Number Estimate link to display the list of accounts.
- Close the Patient List Estimate window.
- Click Save to save your patient list and make it available to models.
Note: If you estimated the number of accounts for your patient list, your estimate is also saved and can be viewed on the Patient Lists tab of the Create Model or Editing Model page.
For more information, refer to the following:
The following table describes each of the fields on the Create Patient List (from Bills) page. The fields are sorted by section and listed in alphabetical order.
Field | Description |
General | |
Name | Name of the patient list |
Facilities | |
Click on a facility to be included | Allows you to select the facilities you want to include in your patient list. This list is limited to the facilities that you have access to. Click a facility name to move it to the list of selected facilities. |
Selected facilities | The list of facilities included in your patient list. Click a facility name to remove it from this list. |
Criteria | |
Admit Date | Date of admission for the account |
Attending Physician NPI | National Provider Identification (NPI) number of the attending physician on the account |
Bill Type | The 3 digit code displayed on a UB that provides specific information about the intent of the claim. The first digit describes the type of facility, the second digit classifies the type of care being billed, and the third digit indicates the sequence of the bill for a specific episode of care. |
Broker | Person(s) or agency who supports the use of the coverage plan and is associated with the claims included in the patient list |
Claim Type | Allows you to limit your patient list to either ICD-9 or ICD-10 claims |
Contract or Product | Allows you to include accounts using a specific contract or product, by facility (multiple selection allowed). The name includes either an A (Admit Date) or D (Discharge Date) at the end indicating if the contract rates are based on the admit date of the contract or discharge date of the contract. |
Detail Service Type | Service type associated with the account. This criteria includes any service type on the account and is not restricted to the primary or highest ranking service type. You can also select the portion of the contract profile where the service type appears, such as Exclusions, Pass-Throughs, Reimbursement, and Stop Loss/Cap. Note: Detail Service Type can only be included as a criteria in your patient list if you selected Bills from the Model patients based on list in the Patient List Source section. |
Diagnosis Code | Diagnosis code associated with the account |
Discharge Status | Patient’s destination upon discharge (home, LTC, etc.), to include or exclude in the search |
DRG | Specific DRG(s) that appear on the claim |
Facility NPI | National Provider Identification (NPI) number for the facility |
Financial Class | Financial class code. |
HCPCS/CPT | HCPCS/CPT code associated with the account. Select Between from the drop down to create a HCPCS or CPT range. Codes are captured regardless if modifiers are present. Fields allow up to 5 alpha numeric characters. |
Hospital Service Code | Hospital service code(s) associated with the claim. |
Message Code | Allows you to include (or exclude) accounts using message codes. |
Operating Physician NPI | National Provider Identification (NPI) number of the operating physician on the account |
Other Physician NPI | National Provider Identification (NPI) number of the physician on the account, other than the attending or operating physician |
Patient Age | Age range for the patient age on the claims. |
Patient Number | Patient account number (for UB claims) or insured ID (for CMS-1500 claims) to include or exclude in the patient list. |
Patient Sex | Patient’s gender |
Patient Type | Patient type assigned to the account: Inpatient/Outpatient |
Patient Zip Code | Patient zip code associated with the account |
Plan ID | Identification code(s) of the coverage plan to include or exclude in the search |
Primary Reimbursement Service Type | The primary reimbursement service type associated with the account |
Procedure Code | Procedure code associated with the account |
Provider Name | Name of the healthcare provider |
Provider Number | Provider’s tax ID number or ten-digit National Provider Identification (NPI) number required on all claims |
Provider State | Use the lookup option to determine if a state is available for a facility prior to executing the patient list. |
Provider Zip Code | Postal zip code for the service provider on the account |
Revenue Code | Revenue code associated with the account |
Service From Date | First date of service rendered to the patient |
Service Through Date | Last date of service for the account |
Severity of Illness | Severity code value associated with the DRG. Use Severity of Illness together with DRG to find accounts based on APR-DRG. Valid values for severity of illness are 1, 2, 3, 4, or blank. |
Submit Date | Date the claim was initially submitted for payment |
Tax ID | Provider’s tax ID |
Taxonomy Code | Provider/specialty type associated with the account |
Total Charges | Dollar amount of the total charges billed on the account |