The RBRVS reimbursement tool lets you calculate reimbursements based on Resource Based Relative Value Systems or Scales (RBRVS), including the following:
- Medicare
- National
- St. Anthony's (Ingenix)
With the RBRVS tool, you can specify a percentage of the reimbursement amount in a particular RBRVS to apply to a specific range of procedure codes. You can use the standard conversion factor or enter any conversion factors applicable to the contract. For example, you can specify that a particular range of codes should be reimbursed at 125% of the Medicare RBRVS, using a conversion factor of 45.5.
In addition, you can also apply a Geographical Pricing Cost Index (GPCI) to further refine your calculations to a specific carrier and locality. By default, the GPCI is determined by the zip code of the location of service from the claim, but you can also override this by entering specific carrier and locality codes to apply to the reimbursement calculation. The GPCI effective date is determined by the effective date entered in the RBRVS tool for a specific code range. If there is no effective date entered for a specific code, the GPCI effective date is determined by the date of service on the claim.
Note: This tool performs its calculations based on Relative Value Unit (RVU) and GPCI master tables so that the reimbursement is calculated as the claim is being repriced rather than being based on a pre-calculated fee schedule.

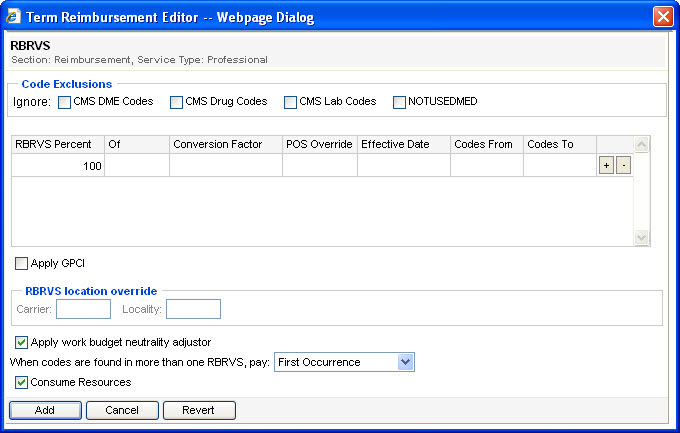
- The Code Exclusions section lets you ignore codes found in the following tables:
- To ignore CMS DME codes, select CMS DME.
- To ignore CMS drug codes, select CMS Drug.
- To ignore CMS lab codes, select CMS Lab.
- To ignore codes in the MPFSRVU table, select NOTUSEDMED.
- The RBRVS Percent field sets the percent of the RBRVS at which the range of procedure codes entered in the Codes From and Codes To fields is reimbursed.
- The Of field lets you select an RBRVS: Medicare, National, or St. Anthony's (Ingenix).
- If you leave the Conversion Factor field blank, the calculation uses the default conversion factor for the selected RBRVS
- The Effective Date field lets you enter the effective date for the RBRVS. If you leave this field blank, the calculation uses the RBRVS that was in effect on the date of service on the claim.
- The POS Override field lets you override the place of service to either a facility or non-facility.
- If you leave the Codes From and the Codes To fields blank, the calculation is applied to all codes.
- A procedure code matches an entry in a lookup table according to standard matching rules.
- The Carrier and Locality fields are only active if you select the Apply GPCI check box.
- If you select the Apply GPCI check box and leave the Carrier and Locality fields blank, the RBRVS tool determines the carrier and locality from the zip code of the location of service from the claim.
- The GPCI effective date is determined by the effective date entered in the RBRVS tool for a specific code range. If there is no effective date entered for a specific code, the GPCI effective date is determined by the date of service on the claim.
- The Carrier and Locality fields must both be blank or both be populated. You cannot enter information in one and not the other.
- The Apply work budget neutrality adjustor check box allows you to apply the 2007 Work Budget Neutrality Adjustor to Medicare and national reimbursements.
The following table describes the fields on the RBRVS reimbursement tool.
Field | Description |
+ | Clicking the plus (+) adds another RBRVS line to the tool and lets you define an additional code range. |
- | Clicking the minus (-) sign removes that RBRVS line from the reimbursement tool. |
Apply GPCI | Selecting this check box applies a Geographical Pricing Cost Index to the calculations performed by this tool. By default, this index is based on the zip code of the location of service from the claim. |
Carrier | This field allows you to enter a specific carrier code to use for the GPCI. If you enter a carrier code in this field, you must also enter a locality. |
CMS DME Codes | Selecting this check box excludes codes in CMS DME tables from pricing with the RBRVS reimbursement tool. |
CMS Drug Codes | Selecting this check box excludes codes in CMS Drug tables from pricing with the RBRVS reimbursement tool. |
CMS Lab Codes | Selecting this check box excludes codes in CMS Lab tables from pricing with the RBRVS reimbursement tool. |
Codes From | The beginning value for your code range. This field is inclusive, that is if you enter a Code From value of 90000, your range begins with code 90000, not 90001. |
Codes To | The ending value for your code range. This field is inclusive, that is if you enter a Code To value of 90000, your range ends with code 90000, not 8999. |
Consume Resources | Selecting this check box consumes resources for the defined code range. |
Conversion Factor | Indicates the conversion factor to apply. Leaving this field blank uses the default conversion factor for the selected RBRVS. |
Effective Date | The effective date of the RBRVS you want to use. Leaving this field blank uses the RBRVS that was in effect on the date of service from the claim. |
Locality | Allows you to enter a specific locality to use for the GPCI. If you enter a locality, you must also enter a carrier. |
NOTUSEDMED | Selecting this check box excludes codes in the MPFSRVU table from pricing with the RBRVS reimbursement tool. |
Of | A drop-down list that lets you select a specific RBRVS., such as Medicare, National, or St. Anthony's (Ingenix) |
RBRVS Percent | Sets the percent of the RBRVS at which the selected range of procedure codes is reimbursed. For example, if you enter 75, all codes within the defined ranges that have not been repriced by another tool are repriced at 75% of the RBRVS. |
When codes are found in more than one RBRVS, pay | Indicates what to do if a particular procedure code is found in multiple RBRVS. You can select First Occurrence to use the first (top) RBRVS listed in the tool, Highest Reimbursement, or Lowest Reimbursement to use the RBRVS that returns the highest or lowest reimbursement of those listed in the tool. |