The Daily Charge Grouping reimbursement tool allows you to define reimbursement for services that are based on a per visit basis (with a single date of service) and where multiple visits can be billed on the same claim.
Infusion therapy is an example of this type of service where the visit is separated from any associated pharmacy, lab, or radiology charges for the visit. If the infusion therapy appears on the claim, the reimbursement is handled differently for the related drug, lab, or radiology charges than if the infusion therapy is not present.
The Daily Charge Grouping term matches contract specifications against claim data. Procedure codes are one of the data types matched, and matching is performed at three points in the process:
- To qualify a day for reimbursement under the term
- To qualify a detail charge or claim revenue item for payment
- To choose a base amount from a fee schedule to calculate payment
Each of these matching processes considers the modifiers associated with a procedure codes to make the correct match. When choosing a base amount from a fee schedule to calculate payment, the reimbursement tool first looks for an exact match of the code plus the modifier. When an exact match is not found, the reimbursement tool then looks for the same code without the modifier for matching purposes. If the code is specified in the tool without a modifier, the code is matched, even when billed with a modifier.
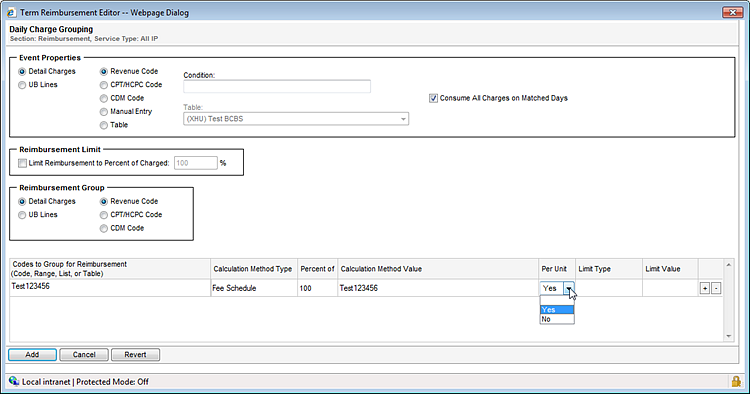
- The Event Properties section of the Daily Charge Grouping tool lets you define the revenue, CPT, HCPC, or CDM code(s) that identify the per visit service or event, such as infusion therapy.
- The remaining sections of the tool let you define the reimbursement for any charges associated with the event.
- To type a value in the Codes to Group for Reimbursement or the Calculation Method Value field, click the field and press Enter without making a selection from the list.
- For more information about specific fields on this page, refer to the Field Descriptions table below.
The following table describes the fields on the Daily Charge Grouping reimbursement tool.
Field | Description |
Event Properties Section | Allows you to define the code(s) that identify the per visit service or event, such as infusion therapy. |
Detail Charges UB Lines | Allows you to determine whether detailed charges or UB lines should be used to identify the event. If you are using a CPT/HCPC code to identify the event, and your facility does not include CPT/HCPC codes on the UB, you must select Detail Charges. |
Revenue Code CPT/HCPC Code CDM Code | Allows you to select the type of code or codes you want to use to identify the event. For example, selecting Revenue Code identifies all codes that you enter in the Condition field as revenue codes. |
Manual Entry | Allows you to mix revenue, CPT/HCPC, or CDM codes in the same condition statement by using three tokens specific to this reimbursement tool. |
Table | Allows you to select a table from the Table field as your condition statement rather than listing specific codes or ranges of codes. |
Condition | Allows you to define the specific code or codes you want to use to identify the event.
|
| With Revenue Code, CPT/HCPC Code, or CDM Code selected, the option button identifies the type of code. You don’t have to enter a token to identify the type of code. For example:
|
| With Manual Entry selected:
Typing CDMProcHas 408 AND CDMRevHas {404-406} requires the claim to include procedure code 408 and either revenue code 404, 405, or 406. |
Consume All Charges on the Matched Days | Provides the option to consume all charges with the same service date as the selected code or codes that identify the event.
|
Reimbursement Limit | Allows you to limit reimbursement to billed charges when using a fee schedule so that reimbursement is capped at billed charges even if the fee schedule amount is greater. |
Limit Reimbursement to Percent of Charges | Provides the option to cap the reimbursement at the code line item level to the billed charges or a percentage thereof, even if the fee schedule amount is greater. |
Reimbursement Group | Allows you to select the type of related codes you want to define reimbursement for. |
Detail Charges UB Lines | Allows you to determine whether detailed charges or UB lines should be used to identify the event. If you are using a CPT/HCPC code to identify the event, and your facility does not include CPT/HCPC codes on the UB, you must select Detail Charges. |
Revenue Code CPT/HCPC Code CDM Code | Allows you to select the type of code or codes you want to define reimbursement for. |
Grouping Details Section | |
Codes to Group for Reimbursement | Allows you to select the specific codes you want to define reimbursement for. This should include any charges associated with the event, such as pharmaceuticals, lab, radiology, and so on.
|
Calculation Method Type | Allows you to define whether to reimburse the selected codes according to a percentage, a flat rate, or a fee schedule. |
Percent of | Allows you to specify a percentage of the fee schedule at the line item level. This field is only available if you selected Fee Schedule from the Calculation Method Type list. |
Calculation Method Value | Allows you to define the specific reimbursement values for the selected code(s).
|
Per Unit | Allows service types using Fee Schedules to price either per unit or once per day.
Note: This option is not available for the Flat Amount or Percentage calculation methods. |
Limit Type | Allows you to define the type of limit or cap, if any, that you want to apply to this reimbursement. You can select one of the following values:
|
Limit Value | Allows you to enter the specific flat rate or percentage to use as a limit or cap for the reimbursement. |
Line Item Opportunity | Displays the variance amount (total line item reimbursement - line item charge) when a code's billed charges are less than the expected line item reimbursement. |