Payor Summary
The Payor Summary display varies, depending on whether the Coordination of Benefits (COB) feature is enabled for your facility. For more information about COB, refer to Coordination of Benefits.
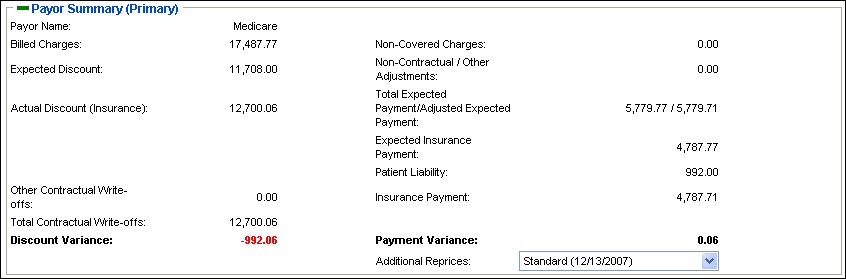
The Primary Payor Summary displays information about the primary payor for the primary account, as shown in the following figure.

The plus (+) and (-) icons let you expand or collapse this section as needed. Hiding the section frees space on the page for you to view the other sections on a page.
In addition, if multiple reprices were performed for this account number, you can use this section to view the details for each reprice. The Additional Reprice field contains a list of all the reprices, by reprice type and service from date, that you can view. To view another reprice, select the reprice type from the Additional Reprice list. Selecting a value from this list updates the Payor Summary, Reprice Summary, and the grid at the bottom of the page with the information for the selected reprice.
The following table describes each of the fields in the Primary Payor Summary. The fields are listed in alphabetical order.
|
Field |
Description |
|
Additional Reprice |
A list of all the reprices by reprice type and service from date that you can view for this account number. This field displays if there are multiple reprices for the account. |
|
Current Reprice |
The type and date of the reprice currently displayed. This field displays if there is only one reprice for the account. |
|
Payor Name |
Name of the payor |
With COB enabled, the Payor Summary displays information about the currently selected payor, as shown in the following figure.
The plus (+) and (-) icons let you expand or collapse this section as needed. Hiding the section frees space on the page for you to view the other sections on a page. By default, this section is collapsed when you enter a page with COB enabled.
The value in the Coordination of Benefits field is a link that opens the Coordination of Benefits Language Definition page that defines the calculation method used. This field only displays for secondary and tertiary payors. For more information about this page, refer to “View the COB Language Definition” on page 148.
In addition, if multiple reprices were performed for this account number, you can use this section to view the details for each reprice. The Additional Reprice field contains a list of all the reprices, by reprice type and service from date, that you can view. To view another reprice, select the reprice type from the Additional Reprice field.
Note: The information that displays for a secondary or tertiary payor in the Payor Summary reflects calculations after COB language is applied. Information in the Reprice Summary and the grid at the bottom of the page displays as if that payor was repriced as primary, prior to the application of Coordination of Benefits language.
The following table describes each of the fields in the Payor Summary with COB enabled. The fields are listed in alphabetical order.
|
Field |
Description |
|
Actual Discount (Insurance) |
Total insurance adjustments for all accounts; Explanation of Benefits (EOB) write-off |
|
Additional Reprice |
A list of all the reprices by reprice type and service from date that you can view for this account number. This field displays if there are multiple reprices for the account. |
|
Billed Charges |
The total charges incurred for the claim or set of claims that have been repriced |
|
Coordination of Benefits Language |
The language type used to calculate a secondary or tertiary expected reimbursement, as specified in the contract profile. This value is a link that opens the Coordination of Benefits Language Definition page that defines the calculation method used. This field only displays for secondary and tertiary payors. For more information, refer to View the COB Language Definition. |
|
Current Reprice |
The type and date of the reprice currently displayed. This field displays if there is only one reprice for the account. |
|
Discount Variance |
Expected Discount minus the Actual Discount |
|
Expected Discount |
Billed Charges minus Non-covered Charges, minus Total Expected Reimbursement |
|
Expected Insurance Payment |
The calculated reimbursement based on the predefined contract terms and conditions and service type definitions in the system and the repriced claims data, minus patient liability |
|
Insurance Payment |
The amount paid by the insurance company |
|
Non-Covered Charges |
The amount of non-covered charges (not disallowed charges) |
|
Other Contractual Write-offs |
Other insurance adjustments not included in the discount variance |
|
Patient Liability |
The amount the patient is responsible for |
|
Payment Variance |
Sum of the payment variance for all accounts associated with this account number, calculated as Total Expected Reimbursement minus the actual payment.
If Patient Liability does not exist, it is calculated as Expected Payment - (Total Insurance Payment + Total Patient Payment).
If Patient Liability exists, it is calculated as Expected Payment - (Insurance Payment + Total Patient Liability). |
|
Payor Name |
Name of the payor |
|
Total Expected Payment/Adjusted Expected Payment |
The calculated reimbursement based on the predefined contract terms and conditions and service type definitions in the system and the repriced claims data |